
Pregnancy is often associated with excitement and anticipation, but for some mothers, it includes medical challenges and emotional strain. A high-risk pregnancy refers to an increased chance of health complications affecting mother, baby, or both. These risks may exist before conception, develop during pregnancy, or emerge around or after childbirth.
Early identification of a high-risk pregnancy and timely access to subspecialised expert care, play a critical role in reducing complications and supporting couples throughout their journey — from preconception, early antenatal care to delivery, recovery and beyond.
What Makes a Pregnancy High Risk?
A high-risk pregnancy often results from a combination of factors, rather than a single cause. Clinicians assess risk by reviewing a woman’s medical history, previous pregnancies, and any complications that arise during the current pregnancy. While being labelled “high risk” can feel daunting, it simply means optimisation, undertaking some essential interventions, managing the mother holistically, closer monitoring and individualised sub-specialised care to prevent complications and to ensure the best possible outcomes.
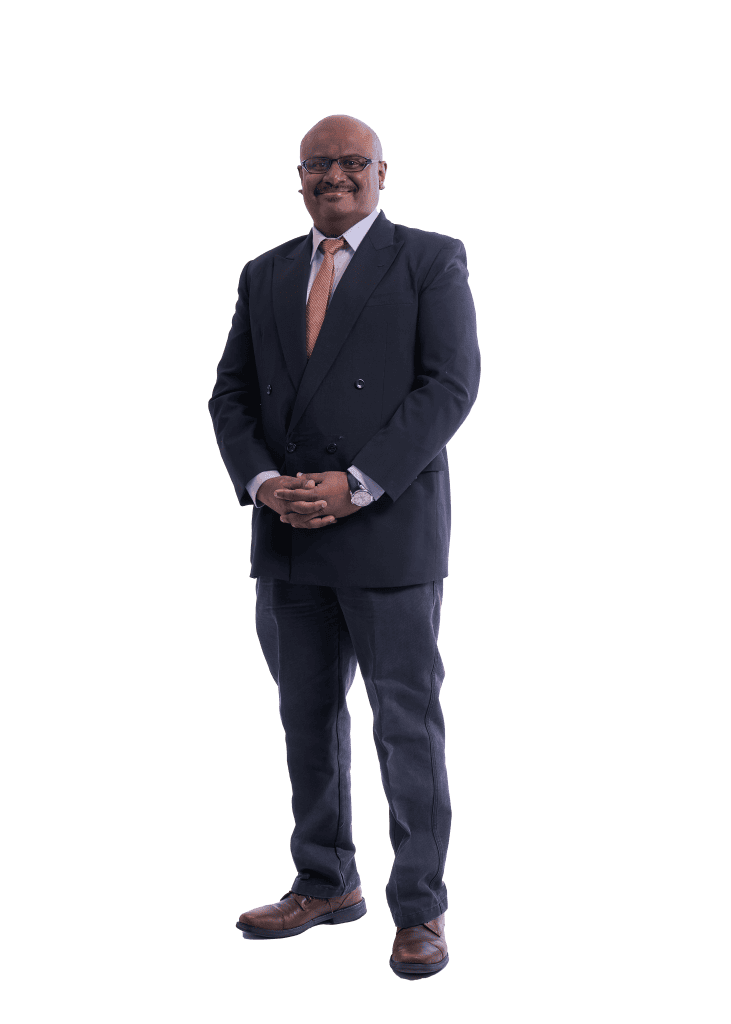
According to Dr Muniswaran Ganeshan, Consultant Obstetrics & Gynaecology (O&G) and Maternal Fetal Medicine sub-specialist at Pantai Hospital Kuala Lumpur, several factors may place a pregnancy in this category. In Malaysia, complications from medical disorders in pregnancies, such as heart diseases, clots, cancers, infections, epilepsy are the leading causes of maternal deaths and complications in Malaysia and in other developed countries.
Hypertensive disorders of pregnancy which is also a common medical disorder in pregnancy affects an estimated 6.5% of mothers who have recently given birth. Globally, preeclampsia occurs in 1–5% of pregnancies and increases the risk of preterm birth, low birth weight, and neonatal intensive care admissions, not forgetting maternal morbidity, complications and death. This can be prevented with early interventions during pregnancy, hence it is essential to see the right expert.
“Pre-existing medical conditions such as diabetes, obesity, heart disease, hypertension, cancers, thyroid disorders, epilepsy, kidney or autoimmune diseases — including mental health illnesses— are key risk factors which define high risk pregnancies,” he explains. “Additional factors include either couples aged above 35, those with genetic conditions, a family history of pregnancy complications, and pregnancies conceived through assisted reproduction, such as IVF.”
Some women may also develop complications, despite having no prior health concerns. These include preeclampsia, thrombosis, gestational diabetes, liver disease, or fetal-related issues such as growth restriction, congenital abnormalities, premature delivery, or stillbirth. “This also includes women with recurrent pregnancy losses,” Dr Muniswaran adds.
“A pregnancy is also considered high risk if there are birth complications, such as a baby born with hypoxia, or maternal complications like trauma or excessive bleeding during delivery.”

Signs and Symptoms You Shouldn’t Ignore
According to Dr Muniswaran, if a patient thinks she is at risk, or has had a previous pregnancy complication, it is important to consult a high-risk pregnancy expert early. While every pregnancy is unique, certain symptoms may signal complications, and warrant prompt medical attention.
These include:
- Persistent or severe abdominal pain, chest pain, palpitations or breathlessness
- Vaginal bleeding or heavy vaginal discharge
- Sudden swelling of the face or hands
- Severe or ongoing headaches
- Changes in vision
- Fever or signs of infection
- A noticeable decrease in fetal movement
- Change in mental state, feeling estranged from the child or suicidal thoughts or self harm.
For women who have experienced pregnancy loss, symptoms can carry emotional weight beyond their physical impact. Sharizat Shaheen Abdullah, who suffered from recurrent pregnancy losses, shares that every warning sign brought back memories of her past losses.
“The most challenging symptoms for me were recurrent bleeding, the fear of cervical incompetence, and the emotional trauma linked to my previous second-trimester loss,” she says. After three miscarriages, her fourth pregnancy was classified as high risk. “Every episode of spotting immediately brought back memories of losing my third baby.”

Managing a High-Risk Pregnancy
Managing a high-risk pregnancy requires a balance of medical monitoring, lifestyle adjustments, and emotional care. Drawing from his clinical experience, Dr Muniswaran recommends the following approaches:
- Prioritise preconception health
Optimising health before pregnancy, such as optimising weight before pregnancy, helps to reduce risks. This includes the health of both parents - Consult the right specialist early
Early specialist care allows risks to be identified and managed safely. See a maternal medicine expert if you have a high risk pregnancy. - Use appropriate medical interventions
This may include low-dose aspirin for preeclampsia prevention, and targeted monitoring for heart conditions. - Take a holistic, continuous-care approach
High-risk pregnancies benefit from coordinated care before, during, and after pregnancy. - Look beyond scans alone
Close monitoring, medication, and timely intervention are essential if you have a high risk pregnancy. - Plan delivery based on individual needs
Not all high-risk pregnancies require caesarean delivery; safe vaginal birth is possible with expert care. - Focusing on the 4th trimester – complications which may occur after childbirth. The risk does not end at childbirth and it is not a time to be confined from seeking healthcare.
- Interpregnancy care – staying healthy in between pregnancies is important to prevent future complications.
Women with high-risk pregnancies typically attend frequent antenatal visits and undergo regular ultrasounds and specialist reviews. Emotional reassurance and clear communication are equally important.
“This pregnancy was managed with much closer and more cautious monitoring,” recalls Sharizat, who delivered her son in 2022. “Instead of rushing into procedures based on fear, my maternal fetal medicine doctor assessed my condition carefully and only intervened when it was truly necessary, ensuring precision and individualised care.”
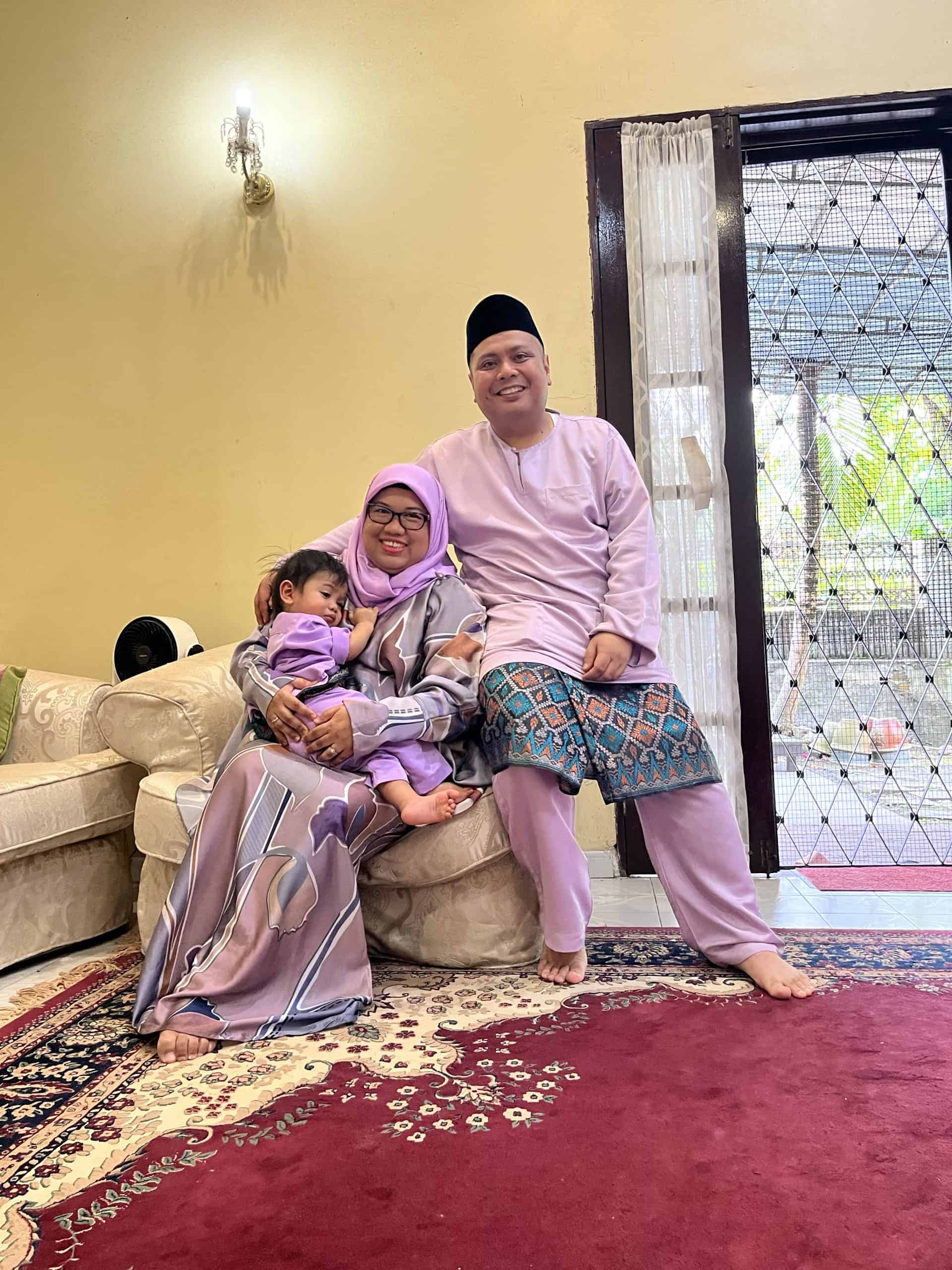
Her journey included an emergency cervical cerclage, infection treatment, gestational diabetes management, low haemoglobin levels, and a COVID-19 infection at 22 weeks. “The maternal fetal medicine team worked as a unit, led by the maternal medicine expert, and I felt heard, supported, and safe throughout the journey.”
She also credits her family for providing essential emotional strength. “My husband was my emotional anchor. My parents and in-laws supported every restriction and prayed constantly. Their presence gave me the strength to endure the most frightening moments.”
Hope, Healing and Next Steps

A high-risk pregnancy can feel overwhelming, but with early intervention, close monitoring, and the right support, many women go on to deliver healthy babies. In Malaysia, maternal health outcomes have improved following the COVID-19 pandemic, with the Maternal Mortality Ratio declining to 26.0 per 100,000 live births in 2022 and 25.7 in 2023 — reflecting continued progress in maternal care as we aspire towards improved standards, quality and safe motherhood. Most tertiary hospitals have maternal fetal medicine subspecialists while a few hospitals have dedicated maternal medicine experts.
“My advice to expectant mothers facing high-risk pregnancies is to remember that you are stronger than you think,” Sharizat shares. “A high-risk diagnosis does not mean the end of hope — it means you need closer care and more compassion for yourself. With patience, faith, and support, a difficult season can also become one of the most meaningful chapters of your life. See the right expert, a maternal medicine expert”
By Desiree Kaur
This is a sponsored post by Pantai Hospital Kuala Lumpur.
Dr Muniswaran Ganeshan specialises in managing high-risk pregnancies such as recurrent miscarriages, IVF, medical complications in pregnancy, multiple pregnancies, and preterm birth prevention. He contributes to national maternal health through guideline development, confidential enquiries into maternal deaths, medical education and is a frequent speaker at national and international conferences. He has led numerous organisations, as the president of the Obstetricial and Gynaecological Society of Malaysia (OGSM) and the founding president of the Malaysian Obstetric Medicine Society (MOMS).
PHKL provides multidisciplinary care for high-risk pregnancies, supported by maternal–fetal medicine specialists, obstetricians, neonatologists, and specialised nurses. With personalised care plans and close monitoring, the hospital supports both medical safety and emotional well-being throughout the pregnancy journey.
To find out more about their integrated obstetrics and gynaecology offerings, book an appointment at +603 2296 0888 or follow PHKL on Instagram, Facebook and Tik Tok for updates.










